The statutory health insurance in Germany at a glance
55 minutes read. Get yourself a cup of coffee! ☕
Basic information on benefits, contributions, and choice of insurance fund in Germany
Statutory health insurance means the free choice of doctors and medical care with a high-quality standard. It also implies redistribution from high-income to low-income earners, from men to women, single people to families, and employed people to pensioners. Statutory Health Insurance (SHI), introduced in 1883, has over 51 million members. Including the non-contributory family members, there are more than 70 million. With an expenditure volume of around 240 billion euros, Germany is one of the world’s leading countries in healthcare costs.
BARMER – Get state health insurance in Germany

Personal health is a precious commodity. Health care and access to the best medical care are key to our quality of life. That’s why BARMER is setting a new standard in healthcare – offering its members award-winning benefits and a wealth of additional services.
BARMER gives you access to one of the best healthcare systems in the world, with German hospitals and doctors of the highest quality. As a patient, you can even choose the doctor or specialist you want to see.
Health insurance, long-term care insurance, accident insurance, pension insurance and unemployment insurance are mandatory in Germany. Around 9 million members place their trust in BARMER. You have many reasons to do so.
Online application BARMER – How it works
As soon as you know that you will move to Germany we can start your process – already in your home country.
- Complete the BARMER application form while simply click through this link: Online application
- BARMER will send you a notification that they received your application. Within 24 hours you will receive the membership confirmation from BARMER for VISA, your employer, and yourself. They immediately apply also for your social security number.
- BARMER will ask you for a photo for your electronic health insurance card. BARMER will upload the photo for you as a service.
Your advantages as a BARMER member
During your working life, you may face all kinds of challenges. With BARMER, you can be sure you’re in safe hands with comprehensive health protection. BARMER works with the best doctors, whose health and treatment plans are particularly varied and flexible. Digital offerings, such as the BARMER app, support you in your everyday life, improve your health and enhance your work-life balance.
- The best medical care and expertise, nationwide
- 100 percent reimbursement of the costs for travel vaccinations
- Naturopathic and alternative medicine
- 24/7 Teledoctor
- 7Mind – one year for free
- The BARMER App – manage all important communication from wherever you are
- Rest well with our sleeping aid
- Receive a payout of up to 100 euros or other attractive bonuses each year:
- Optional tariff – up to 100 euros cashback annually
- Lifelong learning – allowances for health-promoting courses up to 200 € a year
How much does BARMER cost 2022
For employees: The general contribution rate in 2022 is 14.6 percent of your gross monthly earnings. BARMER’s additional individual contribution rate is 1.5 percent. This means that BARMER members benefit from a consistently high quality of benefits and excellent customer service.
For students: If you are younger than 25, you are usually automatically covered by your parents’ family insurance – free of charge, of course. Are you older or do you earn more than 470 euros per month as a working student? Then you need your own health and nursing care insurance for students. BARMER offers this for as little as 111.07 euros per month.
How do I pay for my insurance?
Employees: A certain percentage of your gross income is automatically deducted.
Students: You can either transfer the contribution yourself or we will debit it from your account. The contribution is always debited on the 15th of the following month.
TK – Get state health insurance in Germany

You are looking for a health insurance company that offers you more than the usual standard? You want a partner that focuses on your interests and needs from the very beginning when it comes to your health?
In that case, Techniker Krankenkasse (TK) may be just the right choice for you. TK is a modern healthcare provider where strong benefits, expert advice and convenient service are closely linked.
As a public corporation, TK does not operate for profit, nor is it beholden to shareholders. They see themselves as representatives of the interests of the insured. Their goal is to ensure that policyholders get the most out of their premiums.
Online application TK – How it works
Make sure that you are covered by health insurance from your first day in Germany. To become a member of the health insurance immediately, please proceed as follows:
- Fill out the online application form
- We will immediately send you a confirmation of your application for membership. If necessary, submit the required documents to us.
- We will forward everything to TK.
- After your documents have been checked, you will receive confirmation of insurance from Techniker Krankenkasse.
- You can upload your passport photo online. To do this, you will need a 10-digit number, which you will receive automatically from TK as soon as your membership application has been received by TK.
Your advantages as a TK member
TK was named the best health insurer in Germany by Focus Money 2022. ➠ Source:
In 2021, techniker kasse was also named Germany’s best health insurer for students by Fokus online. In this video, you can find out which advantages TK has specifically for students.
- free choice of specialist and dentist – provided he or she is licensed as an SHI-accredited doctor
- Treatment in approved hospitals
- cost absorption for approved alternative medicine
- medical check-ups
- health insurance cover when traveling to other EU member states
- TK-ReiseMediCall – for example, if you need information about vaccinations
Do you have further questions about TK health insurance in Germany?
The TK team will be happy to answer your questions personally. You can reach them around the clock, 365 days a year.
How much does TK cost 2022
For employees: Since January 1, 2015, there have been new regulations for contributions to statutory health insurance. Employers and employees share equally in the nationwide uniform contribution rate of 14.6 percent.
In addition, each health insurance fund can levy an individual additional contribution, which must be borne solely by the insured person. At TK, the additional contribution in 2022 is 1.2 percent, which is lower than the statutory average of 1.3 percent.
For students: If you have not yet completed your studies but have already reached the age of 30, you can continue to insure yourself with TK. You pay the minimum contribution for voluntary insurance as long as your income subject to contributions does not exceed 1,096.67 € per month.
Students will pay 166.69 euros per month for continued health insurance from January 2022. The minimum contribution for long-term care insurance is 33.45 euros per month, and 37.29 euros per month for childless persons aged 23 and older.
After your insurance as a student ends, you pay the regular contributions for voluntarily insured persons. They depend on your income.
Solidarity
How much an insured person contributes does not depend on the number of insured persons, age, or individual risk of illness; it depends solely on their economic capacity. The rule is: high income, high contributions – low income, low contributions. The benefits of statutory health insurance are the same for everyone, and those with a meager income are even exempt, in whole or part, from co-payments that the other members have to make. Finally, in contrast to private health insurance, statutory health insurance cannot deny membership to anyone.
All compulsorily insured and voluntary members of statutory health insurance (SHI) enjoy insurance protection, as do their spouses and children within family insurance.
Compulsory insurance
No health insurance? There should be no such thing in Germany. Compulsory insurance is a central principle in the SHI and is based on this solidarity principle: Every person who performs an occupation for remuneration and every trainee is subject to compulsory insurance and must join a statutory health insurance fund. In addition, under certain conditions, other groups of persons are subject to mandatory insurance. These include
- Recipients of unemployment benefit or unemployment benefit II,
- agricultural and forestry entrepreneurs and their collaborating family members,
- artists and publicists,
- young people in particular institutions,
- disabled persons,
- Students up to the completion of their 14th semester and, in principle, up to the age of 30 at the latest,
- pensioners and pension applicants.
Exemption from compulsory insurance is only granted upon application in exceptional cases regulated by law. Since 2009, everyone in Germany has had to provide proof of health insurance.
Employees are exempt from insurance if their annual income exceeds the compulsory insurance limit. Even marginally employed persons are exempt from insurance.

Anyone who would be subject to compulsory insurance after 55 and cannot prove a sufficient connection to the SHI remains excluded from mandatory insurance. Due to many individual provisions, the insurance funds personally assess the insurance obligation in each case.
All residents without coverage in the event of illness, who have no other coverage entitlement and were last covered by statutory health insurance, are included in the compulsory insurance. It also applies to returnees from abroad who were last legally insured in Germany. Furthermore, persons who previously had neither statutory nor private health insurance and who fall within the scope of the SHI because they were in employment, for example, are subject to compulsory insurance.
The contributions
In return, for the promises of benefits, the legislature has imposed a duty to ensure: Every worker who is not marginally employed and whose salary is below the compulsory insurance threshold automatically becomes a member of the statutory health insurance scheme.
Those who receive an income above the compulsory insurance limit are not immediately excluded; they can remain voluntarily insured. The same applies to employees who become self-employed. It is important to note that anyone who wishes to remain a voluntary member must notify their statutory health insurance company within three months of the compulsory insurance period. Otherwise, they will lose their entitlement to membership.
A civil law contract does not establish membership in statutory health insurance. It is legally due to the employed person whose salary is below the compulsory insurance limit, and he does not have to apply for membership but registers.
Every employee owes statutory health insurance a certain percentage of their earned income. The situation is different for voluntarily insured self-employed persons: their entire income is used as the basis for assessment. Those earning little from self-employment may pay less than private health insurance. However, there is a minimum contribution that everyone must pay. A particular advantage of statutory health insurance is family insurance. Spouses with no income and children are automatically covered without a surcharge.
Non-contributory co-insurance
Non-contributory co-insurance (family insurance) is a core feature of statutory health insurance. The spouse or the registered same-sex partner and the children of a member are insured free of charge. However, a prerequisite for family members’ insurance is that they reside in Germany and are not otherwise subject to compulsory insurance, exempt from mandatory insurance, or exempt from compulsory insurance.
Anyone self-employed full-time or exempt from insurance or compulsory insurance on the application cannot be co-insured free of charge. It also applies to spouses and partners during maternity or parental leave if no statutory health insurance existed previously.
Children are generally covered by non-contributory health insurance until the age of 18. If children are not gainfully employed, their family insurance ends when they reach the age of 23. It ends when the child reaches the age of 25 if they are in school or vocational training or are doing a voluntary social or ecological year. In that case, the insurance shall continue beyond 25 for the corresponding period.
Without an age limit, children are also insured if they cannot support themselves due to physical, mental, or psychological disability. The prerequisite is that the disability already existed when family insurance existed.
Children are not covered by non-contributory insurance if only one parent is a statutory health insurance fund member. Still, the other parent and spouse of the member related to the children have an income above the compulsory insurance limit. Their total income is regularly higher than the total income of the member.
Switching between insurances is possible

If you are dissatisfied with your health insurance company, you can change as a compulsorily insured person without any problems. An informal letter without justification is sufficient. Health insurance members can cancel with eight weeks’ notice to the end of the month. It is essential to register quickly with the new insurance company. Those wishing to find a new insurance need confirmation from their old fund, and only then can become the new fund issue a membership confirmation for the employer. In any case, you must remain loyal to the new insurer for 18 months. If the insurer increases the contribution rate or reduces the range of services, every member can cancel the contract with two months’ notice.
The benefits
Every member of statutory health insurance receives the same benefits, and basic medical care is guaranteed in every case. The benefits are subject to the “efficiency principle”: they must be sufficient, appropriate, and economical, and they must not exceed what is necessary.
People with statutory health insurance are entitled to comprehensive medical care, regardless of income and age. The legislator has laid down the basic entitlements to benefits:
- Benefits that serve to prevent and alleviate illnesses, as well as benefits for contraception and abortion
- Benefits for the early detection of diseases
- Help for the treatment of diseases
- However, there is no guarantee of the exact scope of benefits. The legislature may redefine the range of benefits provided by the statutory health insurance funds.
Statutory health insurers can also stipulate additional benefit obligations in their statutes – from travel vaccinations to health courses during vacations. Since competition is increasing in this area, it is worth comparing.
The insurance companies settle directly with the doctor or hospital. The patient does not have to pay anything in advance but does not learn anything about the actual costs incurred. Every member of statutory health insurance can consult a doctor of their choice – as long as the health insurance licenses the doctor. The fees are covered directly by their health insurance.
On the other hand, in the case of prescribed therapy, the patient usually has to pay extra. In the case of medications, a co-payment is due. Medicines for minor health disorders are no longer paid for by the statutory health insurers – whether laxatives, cough syrup, or nasal spray.
In the case of massages or physiotherapy and aids such as bandages or insoles, the insured person bears part of the costs. The statutory health insurance members whose income is meager can be exempted from co-payments under an “excess burden clause.” If the co-payments of chronically ill patients due to the same illness exceed one percent of their gross income per year, they are also exempt from making their payments. One in three patients in Germany is exempt from co-payments!

While the statutory health insurance funds cover dental treatment and maintenance costs, patients pay half of the costs of crowns, bridges, and partial or complete dentures. His contribution is reduced if he can prove extensive prophylaxis over five or ten years.
The health insurance fund covers the costs of inpatient treatment in the hospital in full, without any time limit. However, the freedom of choice of the hospital itself is limited. The physician must refer to the nearest hospital that can provide the required therapy. The insured person receives all medically necessary services and treatment from the physician on duty in the hospital. Only private patients are entitled to a double or single room or treatment by the head physician.
All compulsorily insured members also receive sick pay. Sick pay is paid as an “income replacement benefit” after the employer’s six weeks of continued salary payment to the employed members. Students, family members, and retirees are not eligible for such benefits. Sick pay amounts to 70 percent of gross income and up to 90 percent of net revenue. If this is not enough for the household budget, it is advisable to take out supplementary insurance.
Home care is also included in the benefits financed by the health insurance fund if necessary for medical reasons, and you can avoid hospitalization. Pregnant women and young mothers are entitled to home care or home help if this is required for medical reasons, and no one living in the household can take over the maintenance or care.
And how does the doctor get his money?
The statutory health insurance funds pay a lump sum per insured person to the respective regionally responsible Association of Statutory Health Insurance Physicians (KV). The amount also includes the expenses for co-insured but non-contributing family members (for example, children or non-earning spouses). This lump sum covers the outpatient treatment of an entire family in one year. It does not matter whether the family is large or small; it goes to the doctor frequently or rarely.
The distribution of this “total remuneration” among the individual SHI-accredited physicians is the responsibility of the KV. The problem is that the lump-sum payments for the entire year must be sufficient to cover all medically necessary services for the patients. If more medical services are required than planned, the cost of the physicians’ services does not automatically increase, and it means that physicians bear the risk of illness for the population.

Pharmaceuticals
Pharmaceuticals are therapeutic agents with chemical, herbal, or animal ingredients. Medicines, which until 100 years ago were often prepared by pharmacies as prescriptions, are now mainly sold in pharmacies as industrially produced finished medication. Particularly since the 1940s, considerable progress has been made in drug development, so drug therapy is now very important in treating a wide range of diseases.
Drugs can be divided into different groups: according to their active ingredients (for example, chemically defined substances or plant extracts), according to their area of application (for example, painkillers, sedatives, sleeping pills, or anesthetics), and according to their dosage form (for example, tablets, ointments, injections).
The German Medicines Act (AMG) implements EU-uniform requirements and contains strict specifications for the manufacturing, testing, approval, prescription, and trade of medicines. Drugs with high efficacy and high risk or novel active ingredients are subject to medication and may only be dispensed on medical prescription ([ prescription drugs ]). In addition, some drugs are available without a prescription, namely pharmacy-only medicines that may only be sold in pharmacies (non-prescription medications) and over-the-counter medicines that are also available in drugstores, for example.
In statutory health insurance, every insured person is entitled to a supply of medicines, provided they have been approved in Germany and are available only in pharmacies. Certain drugs may not be paid for by the health insurance funds due to supplementary legal regulations: Drugs to adults to treat minor health disorders, for example, cough syrups for colds, and drugs on the negative list, which are excluded by legal regulation as inexpedient or uneconomical. Medications that focus on improving the quality of life (so-called lifestyle drugs) are also excluded from the SHI benefit obligation, as are non-prescription drugs. A further prerequisite for the health insurance funds’ responsibility to provide benefits is a prescription from a physician.
In inpatient care, patients receive drugs as part of their hospital treatment; no prescriptions are issued.
The attending physician decides on the prescription of the drugs. In outpatient care, the physician issues a remedy if the medication is medically necessary, appropriate, and economical for the treatment and if legal regulations do not exclude the drug. To ensure that the essential medicines are prescribed while simultaneously avoiding unnecessary costs in drug provision, there are special legal regulations to ensure quality and cost-effectiveness.
For example, the associations of SHI-accredited physicians and the state associations of health insurance funds agree on so-called guideline values for the prescription of drugs. Guideline values are average for the prescription of drugs (including dressings and consultation supplies) per year and patient. They are set separately for each group of physicians because prescription costs can vary significantly from one group of physicians to another. With the help of guideline values, the cost-effectiveness of physicians’ prescribing methods can be checked. It is done by the so-called review committees, in which representatives of physicians and health insurance funds are represented with an equal number of votes. Physicians who exceed the guideline amount by a certain percentage can be held liable for the additional costs.
To allow physicians to treat “expensive” patients without fear of recourse, many drugs used to treat certain severe or chronic conditions are exempt from the guidelines. In addition, a physician can claim an above-average proportion of “expensive” patients as a practice specialty, which is then considered separately. Finally, physicians can also agree on a specific guideline size for their practice with the audit committee.
Aut idem regulation-You can get the same drug cheaper
“Aut idem” is Latin and means “or the same.” In pharmacy law, the pharmacist can give you another preparation with the same active ingredient to the patient instead of a drug the physician prescribes. You can save significantly by dispensing lower-priced medications with the same active ingredient.
The preparation must be identical to the prescribed drug in terms of strength and package size, be approved for the same clinical picture, and have the same or interchangeable dosage form (e.g., tablets/coated tablets).
In the SHI-Wettbewerbsstärkungsgesetz, pharmacists must dispense only those drugs for which the patient’s health insurance fund has concluded a discount agreement with the drug manufacturers. It only does not apply if the physician excludes “aut idem” on the prescription.
Reference prices regulate the pharmaceutical market
There are many drugs on the German drug market with comparable effects and, in some cases, identical compositions, but whose prices vary widely. The legislator wanted to prevent statutory health insurance (SHI) from being burdened with the costs of expensive drugs when, on the other hand, inexpensive preparations of equal quality are available. For this reason, fixed drug prices have been in place since 1989 to protect the insured community from excessive drug prices.
Reference prices are the maximum amounts for reimbursing drug prices by the statutory health insurance funds. The health insurance funds do not automatically pay every price, but only a fixed amount: these are set for groups of comparable drugs. Thus, the doctor who wants to prescribe a medicine has the choice between several therapeutically equivalent preparations that he can give you at the expense of health insurance.
If the physician prescribes a drug whose price is higher than the fixed amount, the patient must pay this difference in addition to the statutory co-payment; this also applies to patients exempt from co-payment. In this case, the physician is obligated to inform the patient in advance.
Groups of “comparable” drugs can be formed according to different criteria; therefore, three levels of comparability are distinguished: Level, one reference price group, is created from medications with the same active ingredients. Level 2 reference price groups are formed from drugs whose active ingredients are comparable pharmacologically, in particular chemically, while also concerning their therapeutic effect. Level 3 reference price groups are formed from drugs that are not comparable in their active ingredients but are equivalent in terms of their therapeutic impact.
However, the incentive thus created for innovations on the pharmaceutical market can be undermined: Drugs that merely contain molecular variants of already known active ingredients and have pharmacologically identical or similar effects to the original drug can also be patented. The changes in the mode of action or the form of administration are often very minor, and these drugs often do not represent an improvement in drug therapy. Nevertheless, they are considered “new” and come onto the market at high prices. Such drugs are referred to as “analog preparations.”
So-called fixed drug amounts have been introduced to protect the insured community from excessive drug prices. Reference prices are the maximum amounts for reimbursing drug prices by the statutory health insurance funds. Patent-protected drugs that do not bring about a therapeutic improvement can be included in the reference price regulation under certain conditions. The price level for reference prices is based on the average price of those drugs in the lower third of the price range within a drug group.
Family insurance
Free co-insurance of family members
Family insurance is the free co-insurance of family members in statutory health insurance. If you are a member of a statutory health insurance fund, your children and spouse are insured free of charge if they have no income. Free family insurance also applies to civil partners under the Civil Partnership Act.
Children are always covered by family insurance until they reach the age of 18. Family insurance continues until the child’s 23rd birthday if the child is not gainfully employed. Children are covered by family insurance until their 25th birthday if they are in school or vocational training. If the vocational training is delayed by the Federal Volunteer Service or comparable services, the family insurance continues after the 25th birthday as long as the service lasts.

No age limit applies to children who are unable to support themselves. Family insurance includes biological children, the children of family-insured children, and, under certain conditions, stepchildren, adopted children, and foster children. Co-insured children remain insured free of charge after a divorce, and the previously co-insured partner must arrange their insurance.
Family members who are compulsorily or voluntarily insured cannot be insured as family members. Self-employed family members and civil servants cannot be insured as family members if they carry out their activity as their primary occupation. Children are excluded from family insurance if the spouse of the legally insured contributor is not legally insured. Their salary exceeds the annual income limit (JAEG), and they earn more than the legally insured person themselves. During maternity leave and parental leave, spouses are not covered by family insurance if they were not previously covered by statutory health insurance.
Only dependents in Germany can be insured in the family insurance of a statutory health insurance fund. Students can remain family insured during a semester abroad since their center of life continues to be in Germany. In this case, an intention to return should be evident.
Statutory health insurances
Coverage, benefits, and change of the statutory health insurance
Self-employed persons and freelancers can choose between the general contribution rate and the reduced contribution rate. The contribution rate includes payment of sick pay from the seventh week of illness, and it is 14.6 percent of the income subject to contributions. And the additional fee varies from the health insurance fund to the health insurance fund. Those who forgo sick pay the reduced contribution rate of 14.0 percent plus the additional contribution.
The calculation of the health insurance contribution for voluntary members of statutory health insurance is based on the income earned. However, it is impossible to specify an arbitrarily low value as income. Even those who make little or nothing must pay contributions to the health insurance fund for a fictitious minimum wage.
Self-employed persons and freelancers are assumed to have a monthly gross income above the contribution assessment ceiling of 4837.50 euros per month. Some self-employed and freelancers are financially overburdened even with a reduced rate. The minimum revenue of 1,096.67 euros must not be undercut.
The additional contribution of the health insurance funds
Additional contribution 2022
The contribution rate of the health insurance funds is 14.6 percent, and employers pay half of this. This contribution rate is not sufficient to cover the costs of the health insurance funds. Through the additional contribution, employers and employees make up the financing gap in equal parts. The other fee is calculated as a percentage: Those who earn more pay a higher additional contribution.
All members of statutory health insurance who pay their contribution must pay their health insurance fund an additional fee. Family members insured free of charge, such as spouses or children, do not pay an additional contribution.

For employees, the additional contribution is deducted directly from their wages. Employers and employees each pay half of the extra cost.
Recipients of unemployment benefit II do not pay the additional contribution themselves. The job center pays the general health insurance contribution and the additional contribution rate in the amount of the average additional contribution.
Recipients of unemployment benefits I do not pay the additional contribution themselves, and the Federal Employment Agency pays the additional contribution for this group of people.
Social assistance recipients or primary benefits do not have to pay the additional contribution. The basic welfare or social security office takes over the payment for this group of persons.
Persons with disabilities and persons in Lebenshilfe institutions are not required to pay the additional contribution. The respective institutions or facilities pay the extra fee in the average additional contribution.
Students must pay the additional contribution if they do not have family insurance.
The pension insurance company pays half the additional contribution to this pension for pensioners who receive a statutory pension.
For trainees with a salary of fewer than 325 euros, the employer pays the health insurance contribution of 14.6 percent and the additional contribution in the average additional contribution rate.
Insured persons who complete a voluntary social year, a voluntary ecological year, federal, or a European voluntary service do not have to pay the additional contribution themselves. The same applies to participants in the Voluntary Social Year and the Voluntary Ecological Year. The employer pays both the health insurance contributions and the additional contribution in the amount of the average additional contribution rate.
Insured persons who receive maternity or parental benefits or are on parental leave are exempt from the obligation to pay the additional contribution.
If my health insurance company increases the additional contribution, do I have a special right of termination?
Suppose the health insurance company increases the additional contribution. In that case, all members of these health insurance companies have a special right of termination—the notice period: 2 months to the end of the month.
If a health insurance company decides to introduce or increase the additional contribution, it must inform its members in a letter. The legislator stipulates that the health insurance company must refer in the letter to the special right of termination, the average additional contribution, and an overview of the central association of health insurance companies with the amount of the additional payments of the individual health insurance companies.
If the change to the new health insurance company fails, the old insurance relationship remains in place. Insured persons are, therefore, never left without insurance cover.
Additional contribution and optional coverage
During an ongoing extraordinary termination, you must pay the additional contribution to the health insurance company. With the effectiveness of the termination, a change to cheaper health insurance is possible.
How high is the additional contribution? When does it have to be paid?
The health insurance funds determine the amount of the additional contribution rate independently and individually in their statutes. There is no upper limit for the additional contribution set by the legislator.
The additional contribution is a fixed component of the health insurance contribution and is, therefore, due simultaneously as the health insurance contribution.
Is it worth changing my health insurance company because of the additional contribution?
The additional contribution is undoubtedly a reason to review your insurance relationship. Do the price and service of my health insurance still meet my expectations?
Before changing your health insurance company, you should determine your wishes and priorities. Comparison calculators facilitate orientation.
Today, switching to health insurance companies is easy and hassle-free on the Internet.
Health insurance contribution for the unemployed
Significant differences between ALG I and ALG II (Social benefits in Germany)
For recipients of unemployment benefit I (ALG I) and unemployment benefit II (ALG II, Harz IV) with statutory health insurance, the job center pays the general health insurance contribution and the additional contribution for each health insurance fund in full. Privately insured persons receive a subsidy for the private health insurance contribution, and ALG I recipients can join a statutory health insurance fund, even if they were previously privately insured.
Unemployment benefit I
Those who receive ALG I become subject to compulsory insurance in the statutory health insurance and can switch to statutory health insurance – even if they were previously privately insured. For privately insured persons, receiving unemployment benefits is an opportunity to return to statutory health insurance.
Within two weeks of starting to receive unemployment benefits, those with private health insurance must choose a statutory health insurance fund. The Employment Agency pays the contributions to the statutory health insurance even if no unemployment benefit is paid due to a blocking period. After unemployment, continued insurance in statutory health insurance is possible.
With the entry of the insurance obligation because of ALG I, the private health insurance must cancel the PKV contract at the beginning of the membership in legal health insurance. Exception: Those who are 55 or older and were privately insured for five years before the age limit can no longer switch from private to statutory health insurance. Those affected must then clarify what subsidies can be provided for the private health insurance contribution with the job center. The maximum support from the employment agency for private health insurance is 367.97 euros per month.

Anyone who has been privately insured for at least five years and wishes to remain can be exempted from compulsory insurance in the statutory health insurance system. You must make the application within three months. However, it would be best if you considered this step very carefully.
Unemployment benefit II (ALG II = Hartz IV)
The job center pays the health insurance contributions for all ALG II recipients with statutory insurance. ALG II-insured persons can also change health insurance companies at any time. Those who are privately insured as ALG II recipients also remain privately insured. ALG II recipients cannot switch from private health insurance to statutory health insurance. The job center then clarifies which subsidies can be paid for private health insurance.
Unemployed without ALG I or ALG II
Those insured by law but do not receive unemployment benefits I or II can continue to insure themselves voluntarily. To do this, those affected should contact their health insurance company. Necessary: To keep the contribution bearable, one should directly inform the amount of the expected income.
Inform health insurance fund or health insurance company
The following applies to all those affected by unemployment: inform your statutory health insurance fund or private health insurance company about the change in status. Employers must also report the end of the employment relationship to the health insurance fund, but there may be delays here. Especially those who are voluntarily insured by statutory health insurance should report the change quickly so that their insurance coverage is not jeopardized.
Benefits: What the statutory health insurance funds offer
Many health insurers provide more than required by law.
Legally required health insurance benefits
These benefits are the same for all health insurance companies
People with statutory health insurance are entitled to comprehensive medical care, regardless of income or age. The legislature has stipulated the benefit entitlements:
- Benefits for treating illnesses: Every person with statutory health insurance is entitled to medical treatment that corresponds to the recognized state of medical science.
- Benefits for the early detection of diseases,
- Benefits for the prevention and alleviation of illnesses
- Benefits of contraception and abortion
- Benefits to which every insured person has an unconditional right include, in particular, medical, dental, and psychotherapeutic treatment, the provision of medicines, dressings, remedies and aids, home nursing care, hospital treatment, and benefits for medical rehabilitation.
- Benefits catalog of the statutory health insurance funds
The term benefit catalog refers to the total scope of all benefits provided by statutory health insurance. The services must comply with the efficiency principle, be sufficient, appropriate, and economical, and not exceed what is necessary. There is a restriction on the scope of benefits for treating secondary diseases resulting from unnecessary medical interventions, such as cosmetic surgery or piercing complications.
It is the task of the Federal Joint Committee (G-BA) to specify these framework requirements. It issues guidelines for the various service areas, binding for the participating health insurance funds, service providers, and the insured.
Statutory health insurance funds can also stipulate additional service obligations in their statutes – from travel vaccinations to health courses during vacations. Since competition is becoming increasingly fierce, especially in these other benefits, it is worthwhile to make a comparison.
Principle of benefits in kind
” statutory health insurance funds are billed according to the “material resources principle.” The health insurance companies settle directly with the doctor or hospital, and the patient does not have to pay anything in advance but does not learn about the actual costs incurred. Every member of statutory health insurance can consult a doctor of their choice – as long as the health insurance fund licenses the doctor. The prices are covered directly by their health insurance.
Co-payments
A co-payment is due for medications. Medicines for minor health problems are not covered by statutory health insurance – whether laxatives, cough syrup, or nasal spray.

The insured usually pays around 15 percent of the costs for massages or physiotherapy. For aids such as bandages or orthotics, it is as much as 20 percent. The insured pays the lion’s share of the cost of glasses. The statutory health insurance members whose income is meager (around 11,000 euros a year or less) can be exempted from co-payments. If the co-payments for chronically ill patients exceed one percent of gross income per year due to the same illness, they are also exempt from making their payments. One in three SHI patients in Germany is exempt from co-payments!
While the costs of dental treatment and maintenance are covered in full by the statutory health insurance funds, the patient pays a large proportion of the costs of crowns, bridges, and partial or complete dentures. The personal contribution is reduced if the patient can prove that they have undergone extensive prophylaxis over five or ten years. A large market of private supplementary health insurance policies has been developed to supplement the statutory benefits To cover the cost risk of dental treatment.
Hospital choice
The benefits of inpatient treatment in a hospital include all services required for medical care: medical treatment, nursing care, provision of medicines, remedies and aids, accommodation, and meals. The health insurance company covers the costs of inpatient treatment in the hospital in full without any time limit. The co-payment for inpatient treatment for insured persons is ten euros per day.
However, the freedom of choice of the hospital itself is limited. The physician must refer to the nearest hospital that can provide the required therapy. The insured person receives all medically necessary services and treatment from the doctor on duty in the hospital. Only private patients are entitled to a double or single room or treatment by the head physician. You can close the gap between statutory and private hospital treatment by taking supplementary insurance.
Sick pay
All compulsorily insured employees receive sick pay. Sickness benefit is paid as an “income replacement benefit” after the employer’s six weeks of continued payment of wages to employed, paying members. Students, family members, and retirees are not entitled to such benefits. Sick pay amounts to 70 percent of gross income and up to 90 percent of net revenue. If this is not enough for the household budget, it is advisable to take out supplementary insurance.
Home care is also included in the benefits financed by the health insurance fund if necessary for medical reasons, and you can avoid hospitalization. Pregnant women and young mothers are entitled to home care or home help if this is required for medical reasons, and no one living in the household can take over the care or provision.
Health insurance coverage
All compulsorily insured and voluntary members of the statutory health insurance (SHI) and their spouses and children within non-contributory co-insurance (family insurance) enjoy health insurance coverage. In Germany, the following groups of persons are generally subject to compulsory insurance: employees with wages above the marginal earnings threshold and up to the point where the mandatory insurance threshold is exceeded in three consecutive calendar years, trainees, interns, pensioners, students, self-employed farmers, artists, disabled persons, recipients of income replacement benefits (e.g., unemployment benefits) under certain conditions. If these conditions are met, they are compulsorily insured by law and must join a statutory health insurance fund of their choice.
All residents without coverage in the event of illness who have no other coverage entitlement and were last covered by statutory health insurance are included in the compulsory SHI insurance. It also applies to returnees from abroad who were last legally insured in Germany. Furthermore, persons who previously had neither statutory nor private health insurance and who fall within the scope of the SHI because they worked as employees, for example, are subject to compulsory SHI insurance.
Preventive medical checkups
Not perceived to a sufficient extent

Everyone with statutory health insurance has a right to free preventive medical checkups. Screenings focus on diseases that can be treated well if detected early. These include the most common causes of death, cardiovascular diseases, and tumors. Disease and cancer screening have been part of the benefits catalog of the statutory health insurance system (SHI) since the 1970s.
The number of those who use such examinations is low: only under 50 percent of all women (aged 20 and over) regularly go for early cancer detection, and among eligible men (aged 45 and over), the figure is not even 20 percent. Only 17 percent of all women and men take advantage of having a health checkup every three years from 35.
Here is an overview of the preventive examinations paid for by the statutory health insurance funds:
- Early detection of cancer
- Genital examination (annually) for cervical cancer in women aged 20 and older
- Breast examination (annually) for women aged 30 and older
- Mammography screening (every two years) in women 50 years of age and older until the end of 70 years of age
- Prostate examination, genital examination (annually), palpation of lymph nodes in men from the age of 45 years
- Full-body examination of the entire skin in women and men from the age of 35
- Colon and rectal examination (annually), test for hidden blood (annually until age 54) in women and men from age 50, men from age 50: Two colonoscopies at 10-year intervals, test for hidden blood every two years, women age 55 and older: Two colonoscopies at 10-year intervals, test for hidden blood every two years
- Skin cancer screening every two years starting at age 35
- Health checkup
- Check-up (every three years) for women and men from 35: You can receive a full-body exam with blood pressure measurement, blood tests to determine blood sugar and cholesterol levels, urinalysis, and a detailed discussion with the physician.
- Preventive dental examinations
- Examination for dental, oral, and maxillofacial diseases (once per calendar half-year) for girls and boys aged 6 to 18 years, up to 6 years: three examinations
- Treat yourself to preventive dental examinations (once per calendar half-year) for women and men from 18. Even if tartar removal, X-ray examination, or sensitivity test was performed in the same session.
- Protective vaccinations
- Protective vaccinations are part of the benefits catalog of statutory health insurance. In addition, health insurance companies may cover the costs of certain travel vaccinations.
You can get regular vaccinations for infants, children, and adolescents, which every child should receive: Hepatitis B, diphtheria, TetanusTetanus, poliomyelitis (polio), Haemophilus influenzae type B (Hib.) infection, pertussis (whooping cough), measles, mumps, rubella, varicella, human papillomavirus for girls between 12 and 17 years of age.
Booster vaccinations (regulated differently in the statutes of the health insurance companies), which should be refreshed in adults or made up for if the primary vaccination is missing: Diphtheria (recommended every ten years), Tetanus
Indication vaccinations (regulated differently in the statutes of the health insurance funds) in case of increased risk of persons and members of a certain age or risk groups: Influenza (standard vaccination for persons 60 years of age and older), pneumococcal infection (routine vaccination for persons 60 years of age and older), early summer meningoencephalitis (TBE), Haemophilus influenza type B (Hib.) infection, infectious hepatitis A and B, rabies, meningococcal infection, poliomyelitis (polio), varicella, rubella, pertussis (whooping cough)
Pregnancy checkup

A pregnancy checkup includes care during pregnancy and after delivery. It is to examine and advise the pregnant woman, for example, about health risks or nutrition. Doctors, midwives, and health insurance companies work together. Preventive services include:
- Detection and monitoring of high-risk pregnancies
- Ultrasound diagnostics
- Examination for gestational diabetes
- Examination for HIV
- Further blood tests for infections
- Examination and consultation of the woman in labor
- Chlamydia screening
Women aged 25 can receive annual screening to prevent genital Chlamydia trachomatis infection. The most common sexually transmitted bacterial disease can lead to unwanted infertility, pregnancy complications, and neonatal infections.
The doctor can detect abdominal aortic aneurysms early
Men 65 years and older: Your doctor can give you a yearly ultrasound examination to detect abdominal aortic aneurysms.
Child and adolescent examinations
Children and adolescents up to 18 are exempt from the practice fee. The statutory health insurance (SHI) covers several early detection and preventive measures for children and adolescents. Immediately after the child’s birth, the parents receive an examination booklet for children in the hospital or the pediatrician’s office, and it is listed precisely when which examination is due.
Your children are entitled to the U examinations (examinations for the early detection of diseases in children) for girls and boys from birth to six: ten checkups in the first six years of life, starting immediately after delivery (U1 to U9). The U7a examination in the 34th to 36th month of life is new.
J examinations (youth health examination) for girls and boys between the completed 13th and 14th years of life (± one year).
Screenings for children and adolescents
Screenings accompany children in their development
Screenings accompany children’s development, which is remarkably rapid in the first years of life. For this reason, a dense network of preventive examinations has been established for this phase of life in particular. Immediately after the child’s birth, the parents receive a booklet for preventive medical checkups at the hospital or the pediatrician’s office.
U1, after birth: The first newborn examination occurs immediately after birth. This preventive examination detects life-threatening diseases and malformations that must be treated immediately. Breathing, heartbeat, signs of maturity and skin color are checked. On days 2-3 of life, extended newborn screening is performed to detect inborn errors of metabolism and endocrine disorders. By day 3 of life, newborn hearing screening to catch bilateral hearing disorders supplements postnatal screening.
U2, 3rd-10th day of life: The U2 screening is designed to detect congenital disorders and significant health risks in the newborn. It occurs between the 3rd and 10th day of life and includes a thorough examination of organs, sensory organs, and reflexes.

U3, 4th-5th week of life: In the 4th-5th week of life, the doctor checks whether the infant’s reflexes, motor skills, weight, and reactions are age-appropriate as part of the U3 screening examination. At the same time, he examines the organs and hip joints for hip dysplasia and dislocation. The doctor asks about the drinking, digestion, and sleeping behavior during the check-op.
U4, the 3rd-4th month of life: To determine whether the infant is developing and moving in an age-appropriate manner, an examination of the organs, sensory organs, sexual organs, and the skin takes place in the 3rd-4th month of life. The doctor examines the growth, motor function, and nervous system.
U5, the 6th-7th month of life: the doctor checks whether the infant moves and develops according to age. He examines the sensory organs, sexual organs, skin, growth, motor function, and nervous system.
U6, the 10th-12th month of life: Between the 10th and 12th months of life, the examination of the organs and sensory organs, especially the eyes, occurs. The doctor checks motor skills, speech behavior, interaction, and the musculoskeletal system.
U7, the 21st-24th month of life: During the examination in the 21st-24th month of life, the doctor detects visual disorders, tests the speech development, and the fine motor skills and body control of the toddler.
U7a, towards the end of the 3rd year of life: The doctor examines whether there is a visual disorder and whether speech development is age-appropriate. During an examination between the 34th and 36th month of life.
U8, towards the end of the 4th year of life: the dental status, speech development, pronunciation, and behavior, and the examination of mobility and coordination skills occur in the 46th – 48th month of life. The doctor examines the child’s reflexes and muscle strength.
U9, towards the end of the 5th year of life: To detect any diseases and maldevelopments before the child starts school, the doctor examines the child’s motor skills, hearing, vision, and speech development between the 60th and 64th month of life.
U10, at ages 7 to 8: U10 is an additional screening examination designed to close the gap between U9 and U11. It is thus the screening examination for elementary school children. Here you can find more information and health insurance companies that cover the costs of the U10 screening.
U11, at the age of 9 to 10: U11 is an additional screening examination. All health insurance companies do not cover the costs. It focuses on School performance and socialization disorders, dental and jaw abnormalities, sports promotion, and media behavior that is harmful to health. Here you can find more information and health insurance companies that cover the costs of the U11 screening.
J1, age 13 or 14: In the 13th or 14th year of life, the doctor examines organs and the skeleton’s general health and growth development. They check the status of vaccinations, the stage of pubertal development, mental development, and the occurrence of psychological abnormalities. The adolescent answers questions regarding school performance problems and health-threatening behavior such as smoking or the use of alcohol and drugs. Based on the individual risk profile, the physician advises the adolescent on how to avoid behavior that is hazardous to health.
J2, at age 16 to 17: The J2 is an additional screening examination, and all health insurance plans do not cover the cost. Areas of focus: Puberty and sexuality disorders, career choice and socialization, trusting conversation with the doctor about health problems – even without parents. Here you can find more information and health insurance companies that cover the costs of the J2 screening.
Preventive dental care for children and adolescents
New as of July 2019:
6-34 months of age: Three dental screening exams educate parents about the causes of oral disease. The application of fluoride to harden tooth enamel for children of this age is included in the statutory benefits catalog of the health insurance funds.
3-6 years of age: Early dental checkups for dental, oral, and maxillofacial diseases with a detailed examination of the oral cavity, assessment of caries risk, advice for the child and parents on oral hygiene and nutrition, motivation for prevention, and recommendation of suitable fluoridation agents.
6 – 18 years of age: preventative services: Survey of oral hygiene status, education of the insured and parents about causes of disease and their prevention, local fluoridation and sealing of caries-free fissures and pits of molars. The semi-annual examinations are entered in a bonus booklet from twelve.
Protective vaccinations
Statutorily insured persons are entitled to protective vaccinations
Protective vaccinations are mandatory benefits of statutory health insurance. Exceptions are special vaccinations for private or professional trips abroad. However, some health insurance companies also cover these travel vaccinations.
Protective vaccinations have multiple benefits:

- They protect the vaccinated against infectious diseases with no or only limited treatment options, which can be severe—for example, Measles, meningitis and hepatitis, Tetanus, or whooping cough.
- They protect the unborn child by helping to prevent damage from infections during pregnancy. Example: rubella.
- They protect against the spread of infections in the population. The prerequisite is that enough people are vaccinated.
- The details of the vaccinations covered by the statutory health insurance funds are determined by the Federal Joint Committee (G-BA). It is based on the Standing Commission on Vaccination (STIKO) recommendations at the Robert Koch Institute (RKI). The STIKO is the expert committee developing recommendations for implementing protective vaccinations following the Infection Protection Act.
List of protective vaccinations that are covered by statutory health insurance:
Cholera: only in exceptional cases (e.g., a business trip to a country that requires vaccination).
Diptheria: at the age of 2, 3, and 4 and between the 11th and 14th month of life. Booster vaccination every ten years.
TBE (tick-borne encephalitis): only for people living in risk areas, not for vacation trips.
Yellow fever: only in exceptional cases (e.g., a business trip to a country that requires the vaccination)
Shingles: for all over 60 and persons with increased health risk over 50.
Haemophilus influenzae type B: at the age of 2, 3, and 4, and between the 11th and 14th month of life, or later if risk factors are present
Hepatitis A (HA): in cases of sexual behavior with a high risk of infection and for specific risk groups (for example, frequent handling of blood components, employees in welfare institutions, asylum seekers’ homes, etc.)
Hepatitis B (HB): at ages 2, 3, and 4, and between 11 to 14 months of age, and for high-risk groups
HPV (protection against cervical cancer): girls between 12-17 years of age
Influenza (protection against influenza): standard vaccination from age 60 and for risk groups
Measles: 11-14 months of age, before the end of the 2nd year of life, and for risk groups
Meningococcus: immunization in the 2nd year of life, as well as for risk groups (especially during more extended professional/study-related stays abroad)
Mumps: from 11 months of age and before the end of the 2nd year of life, as well as for risk groups (especially people who are frequently surrounded by children)
Pertussis: at ages 2, 3, and 4, and between 11 to 14 months. Booster at age 5-6 and between 9-17 years. In some cases, also for women of childbearing potential and other persons who have frequent contact with newborns.
Pneumococcal: At ages 2, 3, and 4 and between 11-14 months. Repeat vaccination for persons over 60 years of age and for risk groups (for example, immunodeficiencies and chronic diseases).
Poliomyelitis: At ages 2, 3, and 4 and between 11 to 14 months. Booster vaccination between 9-17 years of age. Renewed entitlement for all who have not received a primary vaccination and if risk factors are present (especially when traveling abroad or dealing with people from polio risk areas).
Rubella: Between 11-14 months of age and before the end of the 2nd year of life. Also, for risk groups (especially contact with small children).
Tetanus: At ages 2, 3, and 4, between 11-14 months. Booster at age 5-6 years and 9-17 years. Every ten years after that.
Rabies: Only during professional/study-related travel to risk areas.
Tuberculosis: currently no vaccination.
Typhoid fever: only for occupational/study-related travel to risk areas

Varicella: Between 11-14 months of age and before the end of 2 years of age. Standard vaccination for unprotected 9- to 17-year-olds with no history of varicella. Also, for high-risk groups (for example, frequent exposure to young children or severe neurodermatitis).
Standard vaccinations for infants, children, adolescents:
- Diphtheria
- Tetanus
- Poliomyelitis (polio)
- Haemophilus influenzae type B
- Pertussis (whooping cough)
- Hepatitis B
- Measles, mumps, rubella (MMR)
- Varicella
- Pneumococcal infection
- Meningococcal infection
- HPV (human papillomavirus for young women)
- Rotaviruses
- Booster vaccinations for – children and adolescents
- 2 x diphtheria
- 2 x tetanus
- 2 x pertussis (whooping cough)
- 1 x poliomyelitis
- Polio
- Pertussis (whooping cough).
Health insurance companies pay for the vaccination of pregnant women and people near the pregnant woman.
Benefits for children and adolescents
Statutory health insurance offers more to children
Children and adolescents are entitled to several health benefits more than adults are. For children and adolescents under 18, the statutory health insurance funds pay for preventive medical checkups, vaccinations, orthodontic treatment, dental examinations, and aids such as eyeglasses.
Preventive medical checkups for children and adolescents
The statutory health insurance funds regular preventive examinations for children and adolescents to detect developmental delays, health problems, and diseases in good time. Parents do not have to make any additional payments. The examinations focus on physical and mental developments and vaccination status between the child’s birth and sixth birthday. Between the child’s 13th and 14th birthdays, an adolescent examination examines the adolescent’s developmental and emotional state.
Vaccinations for children
The statutory health insurance funds pay for eleven protective vaccinations, which are to be carried out on fixed dates. These include vaccinations against diphtheria, Tetanus, polio, hepatitis B, and whooping cough. For young women, vaccination against cervical cancer is also covered by statutory health insurance. The necessary booster vaccinations are also paid for by statutory health insurance.
Orthodontic treatments
If there is a medically justified indication, orthodontic treatment for children and adolescents under 18 is covered by statutory health insurance. It means that biting, chewing, speaking, or breathing must be significantly impaired or threatened by malocclusion of the teeth. If this is the case, the SHI will cover 80 percent of the costs incurred. The statutory health insurance does not contribute to the charges if the impairment is minor or the treatment is cosmetic.
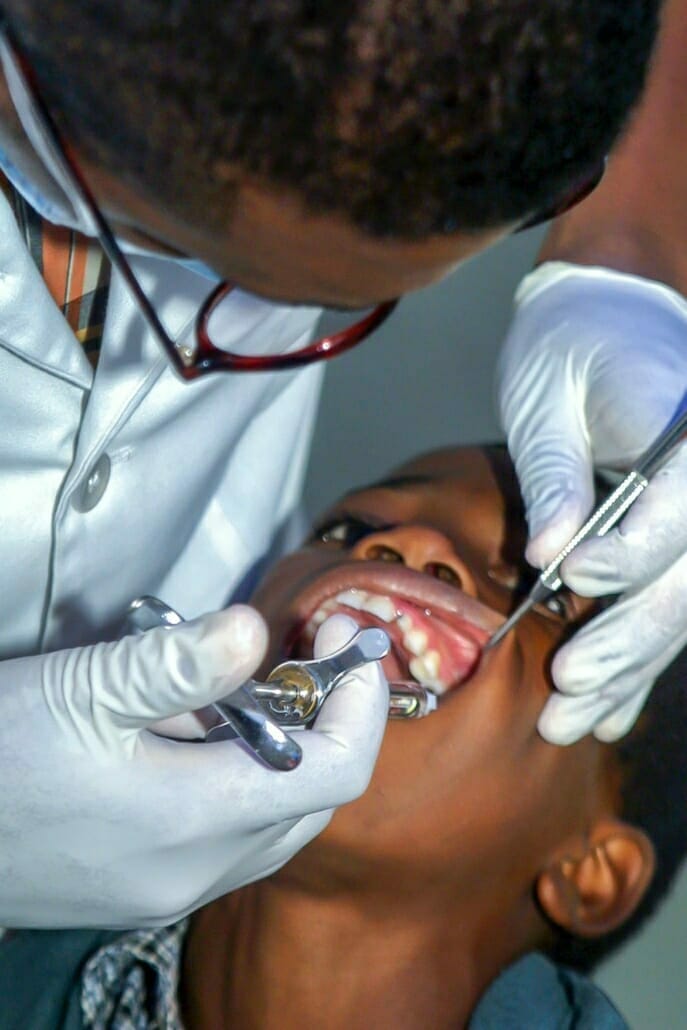
Dental treatments
Children between the ages of three and six can be examined three times a year for dental, oral, and maxillofacial diseases at the expense of the health insurance company. Six to 18-year-olds can be checked twice a year. Examination certificates are required from the twelfth year, recorded in a bonus booklet, and guarantee higher subsidies for dental prosthesis treatments. Dental services include fissure sealants, fluoridation, and oral hygiene consultations. Services such as professional dental cleanings are often covered by statutory health insurance as a benefit but are not part of the legally required benefits catalog.
Entitlement of glasses for children and adolescents
Children and adolescents are entitled to glasses until the age of 18. From 14, there is a renewed entitlement only if the visual acuity changes by more than 0.5 diopters. Children are entitled to plastic lenses if they are of preschool age or younger than 14 and their vision is impaired by more than plus or minus five diopters. Statutory health insurance also covers the costs if plastic lenses are necessary to participate in school sports.
If the child becomes ill – health insurance benefits
According to the doctor, the statutory health insurance pays a children’s daily sickness allowance for sick children under twelve years of age if necessary care and parents cannot pursue their work. The entitlement to the children’s daily budget is for ten working days per year; if there are several children, the statutory health insurance pays a maximum of 25 working days paid by the statutory health insurance. Higher entitlements apply to single parents; sickness benefits are also paid for children with disabilities after twelve.
Braces
When do braces make sense? What does health insurance pay?
Every second child in Germany wears braces – often due to malocclusions or significant gaps between the teeth. The correction of pronounced malocclusions is covered by statutory health insurance up to 18 – provided it is medically necessary. If dentists advise a visit to an orthodontist, this triggers many questions among parents.
What costs are covered by health insurance?
The orthodontist determines the malposition and submits a treatment and cost plan to the health insurance company. How severe malocclusions are is regulated by the orthodontic indication groups. These range from mild severity (severity 1 and 2) to severe developmental disorders (severity 5). If the malocclusion is in severity grade 1 or 2, it is considered purely aesthetic and is not covered by health insurance.
The orthodontist may offer additional services that parents pay for on their own. Therefore, in any case, parents should consult with their health insurance company before signing a cost commitment. The statutory co-payment of treatment costs for braces is 20 percent, and for siblings treated at the same time, it is 10 percent. After completing the treatment, your health insurance will refund you the paid share.
How do parents get their co-payment for braces refunded?
The orthodontist settles directly with the health insurance company and invoices the parents for the co-payment. If the treatment is discontinued, the co-payment is lost. For this reason, parents should make sure that their children wear loose braces regularly and brush their teeth thoroughly. At the end of treatment, the orthodontist will issue a certificate of completion. Parents submit the bills and the certificate of completion to the health insurance company. If necessary, you must complete an additional application form before the co-payment is reimbursed.
When are braces essential?
Few people have the “perfect” set of teeth by nature. The new teeth often grow crooked if the milk teeth have fallen out. Sometimes a pronounced jaw misalignment is also to blame. Children can grow up happy and healthy even with crooked teeth, but this is not always just an aesthetic problem. Under certain circumstances, malocclusion can become a medical risk and lead to biting, chewing, or speaking disorders. In this case, treatment with braces makes sense to avoid late consequences.
Can I get a second medical opinion?
Absolutely! Especially if expensive additional services are recommended, or healthy teeth are even to be extracted, affected persons and parents should make an appointment with another orthodontist and get a second opinion. Also, if there is uncertainty about whether braces are necessary, another consultation can help. The more information available, the easier it is to decide for or against treatment.
Should children get braces as early as possible?
For a long time, the widespread opinion was: that the earlier, the better. Children often get their first braces before all their milk teeth have fallen out. In the meantime, British scientists have discovered that the treatment result does not change if the treatment is not started until adolescence. The National Association of Statutory Health Insurance Dentists recommends braces only from 10 to 13.

Which braces make sense?
Whether your child gets loose or fixed braces depends mainly on the amount of treatment required. Often, treatment is started with removable braces and continued later with fixed braces. With loose braces, treatment success usually takes much longer. The motivation to wear them is low, and the pull on the teeth is much weaker. Nevertheless, it is well suited for slight tooth misalignments. The constant force with fixed braces achieves better results in a much shorter time.
Are lingual braces worth it?
Lingual braces are very similar to regular fixed braces, except they are placed on the inside. So, lingual braces are almost invisible from the outside and allow for “invisible” teeth straightening. This method is recommended for children and teenagers because they are often afraid of teasing associated with braces. However, health insurance does not cover lingual braces as they are an aesthetic solution. Therefore, the difference in cost compared to traditional fixed braces must be covered by yourself.
How much do braces cost?
Orthodontic treatment is a lengthy process that is individually tailored to medical needs. The cost of braces can vary accordingly. Private add-ons such as tooth-colored brackets and expensive materials promise better comfort and shorter treatment times. However, they do not always make medical sense. The patient must bear such costs, and amounts of up to 1000 euros are not uncommon.
Dentures and fillings
Fixed subsidies for dentures, the most favorable solution for dental fillings
Whether dental crowns, bridges, or dentures – dental prostheses are a benefit of statutory health insurance (SHI). However, the health insurance subsidy of dental prosthesis services does not usually cover all costs: the patient with statutory health insurance has to pay extra. The health insurance funds pay fixed amounts for dental prostheses, so-called findings-related fixed subsidies.
Dentures
Dental prostheses are crowns, bridges, removable dentures, and implants. The health insurance subsidy amount is not based on the treatment method but on the dental findings – the tooth gap that is being replaced or the tooth that needs to be crowned. The health insurance company pays the fixed subsidy based on the results, regardless of whether you opt for a simple or a complex therapy.
Let’s assume that the dental diagnosis is a tooth gap with one missing tooth. In most cases, the missing tooth is compensated by bridge construction. This solution corresponds to the so-called classic restoration. However, patients can also opt for a different, more complex repair, for example, an implant-supported denture that replaces the missing tooth.
Such a solution serves the same purpose but is significantly more expensive than bridge construction. No matter which dental restoration is chosen, the subsidy from your health insurance company remains the same. It is 50 percent of the cost of the standard repair. The benefit increases to 70 to 80 percent if the teeth are regularly cared for and attended annual preventive checkups. Children go for checkups every six months; the dentist confirms this in a bonus booklet.
The patient bears the additional costs for dental prostheses that deviate from the standard treatment. The dentist prepares a free treatment and cost plan before treatment begins. It includes the findings, the standard treatment, and planned dental prostheses in terms of type, scope, and costs. The health insurance company checks the treatment and cost plan before treatment begins. If the treatment is necessary, the health insurance company approves the fixed allowance following the treatment and cost plan findings.
In the past five years, for those who visited the dentist once a year for a checkup, the fixed allowance from the health insurance fund increased by 20 percent. Those who can provide evidence of this checkup for the last ten years will receive a 30 percent higher fixed allowance.
Insured persons who have a low income – for example, recipients of social welfare, unemployment benefit II, or educational grants – receive a fixed subsidy from their health insurance company for the costs incurred for standard care. It means that they receive the standard treatment free of charge.

Dental fillings
The extent to which the statutory health insurance funds cover the costs of dental fillings depends on whether the teeth to be treated are in the anterior region (incisors and canines) or the posterior part. For anterior teeth, the statutory health insurers cover the costs of tooth-colored composite plastic fillings. If patients have special esthetic requirements for the composite filling, such as color optimization, additional charges arise, which the patient must pay himself.
In the case of posterior teeth, the statutory health insurance funds only cover the costs of amalgam fillings in the posterior region. However, amalgam fillings have been prohibited since July 2018 in the dental treatment of deciduous teeth, children under 15 years of age, pregnant women, and nursing mothers. Amalgam may also not be used in cases of amalgam or mercury allergy. In this case, the statutory health insurance companies also cover the posterior teeth’ cost of a composite filling.
All patients can opt for a filling material other than amalgam. Patients with statutory health insurance must bear the additional costs themselves. In such cases, patients with statutory health insurance – after an explanation and consultation with the doctor – conclude an additional cost agreement with the dentist. The patient agrees to pay the additional costs incurred. You can take supplementary dental insurance if you want to protect yourself against this risk.
Eyeglasses and other visual aids
Only in the case of children and severe visual disorders do the health insurance companies pay
Health insurance companies only pay for glasses and other visual aids for children under 18 and those with severe visual impairments. For adults, health insurance pays vision aids for nearsightedness and farsightedness of six diopters or more, astigmatism of four diopters or more, or level 1 blindness on both sides.
Patients must always pay for the spectacle frame. Lenses are subsidized with fixed amounts, and those with statutory insurance must always pay for extras such as anti-reflective coating or tinting of the lenses. Children and adolescents are entitled to glasses, and normal vision is essential for overall development in childhood and adolescence.
In the case of adults, the entitlement to benefits is limited to exceptional circumstances that are medically necessary. Such exceptions exist when insured persons have a severe visual impairment of at least level 1 in both eyes due to their visual impairment or blindness, according to the severity of visual impairment recommended by the World Health Organization (WHO).
As a rule, these insured persons already require magnifying vision aids such as reading magnifiers, telescopic glasses, or electronically magnifying vision aids (screen readers) to reading aids to reading conventional texts. Insured persons with significant visual field defects are also counted among the severely visually impaired and are thus entitled to be provided with visual aids.
Health insurance pays for glasses for nearsightedness and farsightedness from six diopters and astigmatism from four diopters. In addition, there is an entitlement to therapeutic visual aids. These are special lenses and spectacle lenses that serve the treatment of eye injuries or eye diseases.
Beyond the groups, as mentioned earlier, of people, those with statutory health insurance bear all the costs for Billen themselves. A health insurance subsidy for glasses is possible for welfare recipients and seniors with meager pensions. Concerned ones should address their health insurance company. There is one consolation for all those with statutory health insurance: it is still possible to claim the cost of the new glasses in the tax return.
Hospital
It can make sense to take out supplementary insurance
Statutory health insurers cover the costs of all necessary treatment and hospital accommodation. Statutorily insured persons over 18 pay a co-payment of ten euros per day for a maximum of 28 days of stay per year. The hospital settles the co-payment directly with those with statutory insurance.
No free choice of doctor
Statutorily insured patients do not have a free choice of doctor, and the hospital decides which doctor will treat the patient. Those who wish to be treated by the head physician or a specific physician can use this as an additional “optional service.” As a rule, accommodation in a single or double room is also an optional benefit. In both cases, the patient bears the additional costs themselves.
Patients with statutory health insurance who wish to take advantage of optional services can take out private supplementary insurance. This “inpatient private supplementary insurance” then covers the related additional costs of treatment or accommodation.
Free choice of hospital
The right to free choice of hospital is generally available to those with statutory health insurance. It applies not only in emergencies but also to planned treatments. Even if the attending physician refers the patient to a nearby hospital, the insured person can choose another. The only condition: The hospital is approved for treating statutorily insured persons.
In this way, statutory health insurances guarantee their customers a free choice of hospitals. It does not mean that if the insured person has a free choice of hospital, they also have a free choice of doctor in the hospital. In this case, the hospital decides which medical professionals are used to providing medical care to the patient.
The health insurers do not have to bear the additional costs incurred by choosing a further away hospital. Patients who choose hospitals in another state should ask their health insurer beforehand.
Rehabilitation
Recovery of physical, occupational, or social skills
Several medical procedures require systematic and comprehensive rehabilitation, whether after a stroke, heart attack, tumor removal, or hip surgery. Its goal is to help the patient regain or maintain physical, occupational, or social abilities.
Health care is currently divided into primary care (outpatient treatment by physicians in private practice), acute care (inpatient care in hospitals), and rehabilitation.
A distinction is made between three rehabilitation services:
Medical rehabilitation services aim to prevent, eliminate, or prevent the worsening of possible disabilities or the possible need for long-term care.
Vocational rehabilitation services promote the patient’s integration into working life.
Social rehabilitation services promote participation in community life. They aim to help patients cope with everyday demands and reintegrate into their social environment.
In Germany, rehabilitation services are the responsibility of the various social insurance institutions, i.e., statutory health, pension, and accident insurance. All medical rehabilitation is a compulsory service provided by statutory health insurance funds. In addition to a general practitioner’s treatment in a hospital, rehabilitation is an integral part of the treatment chain. For many diseases, only the close integration of this chain ensures optimal care.
The aim of rehabilitation is not only to maintain or improve patients’ physical, occupational, and social performance; it also promotes individual abilities and opportunities to cope with illness and life. Patients learn to behave so that, if possible, further acute disease states do not occur, and chronic disorders can be limited or controlled in their effects as well as likely.
Insured persons can independently select preventive care and rehabilitation facilities that are licensed and certified. However, they must pay any additional costs themselves.

Cure after illness or for preventive care
Apply to your health insurance company for reimbursement
Cures are approved after an illness (rehabilitation) or preventive care measures (prevention). You will be sent to a special cure facility in case of a cure. It is something like a health hotel. You usually get a room for yourself and are subject to particular treatments aimed to help with your symptoms. You may be subscribed to massages, watersports, and psychotherapy sessions. A frequent case is “follow-up rehabilitation”: it is intended to help the patient recover quickly after treatment in the hospital and continue living independently. For this reason, cures are often prescribed after heart attacks or similarly severe illnesses.
A cure can also be approved if there has been no previous hospitalization. Treatments are intended to help manage disease states better or prevent them from worsening. Older people, in particular, have been taken into consideration: they should not be sent to nursing homes too soon but should live in their own homes for as long as possible. The health insurance company will probably approve the application if the doctor proves that a cure serves these goals. However, it has the right to examine the individual case and determine the medically necessary service.
Especially when it comes to covering room and board costs, most insurance companies are somewhat reluctant. It is because rehabilitation should primarily take place on an outpatient basis – for example, in a rehabilitation center near the patient’s place of residence.
Preventive cures(Kur) are to be distinguished from rehab cures. These are aimed at people at risk of illnesses that can be reduced by therapy. However, the health insurance company only covers room and board costs in a few medically justified cases. Parents have it somewhat better. Since April 2007, the health insurance company has been paying for an inpatient mother-child or father-child cure. However, the following also applies: the cure must be medically necessary.
Those with statutory health insurance should first discuss their application for a cure with their doctor. They must clarify whether rehabilitation or preventive cure is necessary from a medical point of view. You can obtain the form for applying for a rehabilitation cure from the doctor. For preventative cures, documents from the health insurance company are usually used. A doctor can prescribe a mother or father-child cure.
Cures for mothers and mother-child (fathers, father-child)

Cures for mothers and mother-child (fathers, father-child) are a mandatory benefit of health insurance. The measures are aimed specifically at the unique needs of mothers and fathers with family responsibilities. During the three-week stays, physical illnesses and psychological complaints are identified and treated within the mother and child cures framework and father and child cures.
In principle, all women (and men) with family responsibilities are entitled to inpatient measures to prevent and rehabilitate mothers (and fathers). Health insurance companies must approve medically necessary cures and thus also mother and child cures.
The contact person is the family doctor or gynecologist who applies for the mother and child cures or father and child cures at the health insurance company. Before applying, the doctor checks whether the patient requires preventive care or rehabilitation, and he also determines both the prognosis and the goal of the measure.
Sickness benefit, children’s sickness benefit, and maternity benefit
Employees and self-employed persons can receive sick pay
In case of incapacity for work, employees receive six weeks of continued payment of wages from their employer. After six weeks, the health insurance fund pays sick pay. After six weeks, a self-employed person can also receive sick pay if they pay the regular contribution to the statutory health insurance.
Members of statutory health insurance funds are entitled to sick pay if the illness makes them unable to work or if they are treated as an inpatient at the expense of the health insurance fund. As a rule, the sickness benefit provided for by law amounts to 70 percent of the regular pay and income previously earned. It means that one-time payments such as Christmas and vacation bonuses are also included in calculating this gross income. However, the legislator has stopped overly creative calculations that inflate gross income. Under no circumstances will more than 90 percent of the net income be paid.
Sick pay is calculated for calendar days and is paid over a more extended period, and it only ends after 78 weeks. These 78 weeks can accumulate within three years for anyone who falls ill again under the same circumstances. These restrictions are intended to prevent sick pay from becoming a permanent pension.
Sick pay for caring for a sick child
Entitlement to sick pay does not only arise when the insured person is ill. Sickness benefits may also be paid for when a sick child is being cared for. However, this only applies if no other person living in the household can supervise, care for or nurse the child. Entitlement to sickness benefit in the event of a child’s illness only exists if the sick child is covered by statutory health insurance.
The period of entitlement to child sickness benefit is ten days for each child and 20 working days for single parents. The double entitlement is intended to ensure that the children of single parents are not treated less favorably than those of married couples. However, there are limits for insured persons with more than two children, and they can take time off from work for 25 (single parents 50) working days per calendar year. Child care sick pay is paid if the child has not yet reached the age of twelve or is disabled and dependent on assistance.
Maternity benefit
Women who are members of a statutory health insurance fund receive maternity benefits from their health insurance fund during the maternity protection. The prerequisite is that the woman is employed or working from home at the beginning of the protection period (six weeks before delivery) or that the employer has permissibly terminated her employment relationship during her pregnancy.
The maternity allowance is the average daily pay for the last three calendar months before starting the protection period, reduced by statutory deductions. The maximum daily maternity benefit is 13 euros. Suppose the average net pay exceeds 13 euros for the calendar day. In that case, the employer must pay an allowance equal to the maternity benefit, and statutory deductions reduce the calendar-day average wage.
Switching: How to join a new health insurance fund

Cancellation not required: simplifying the process of switching health insurers
Switching health insurers has been easier since January 2021. Anyone who wants to change health insurance companies applies to join the new insurance company. The new health insurer informs the old one, and notice of termination is no longer required. The new notification procedure between the health insurance companies replaces the notice of termination.
Who can change health insurance companies?
Anyone who has been a member of their old health insurance fund for at least 12 months can change to any other statutory health insurance fund. If the own health insurance company increases the additional contribution, a special right of termination applies. Switching your health insurance company is also possible within the twelve-month binding period. Family members can change at any time when they are required to be insured.
What notice periods apply when changing health insurance companies?
Anyone wishing to change health insurance companies must observe a notice period of two months to the end of the month. If you apply for membership in January, you will become a new health insurance fund member on April 1. The health insurance companies take care of the correct application of the deadlines. The latest and old health insurance companies compare their data to determine when a change of health insurance companies can occur. The new insurance company informs you about the change date as soon as the data exchange with the previous health insurance company has taken place.
When changing the employer, you can immediately join another health insurance company. Here you aren’t required to adhere to any time limits. Also, the twelve-month connection to the old health insurance company does not exist. This immediate right to choose a health insurance company applies for the first 14 days after starting employment. The same applies to any change of status under insurance law. Anyone who was compulsorily insured and wished to continue to be insured voluntarily can change health insurance funds immediately. Family-insured persons do not cancel their insurance but join the chosen health insurance fund directly when compulsory insurance becomes effective.
Does the new health insurance company have to accept me?
What are the risks of changing health insurance companies?
Your membership with the old health insurance company will only be terminated on the change date if the new health insurance company has confirmed the membership in writing. In plain language, this means that insurance coverage is not jeopardized when changing health insurance companies. There can be no gap in health insurance coverage. If the insurance with the new health insurance company does not materialize, one automatically remains insured with the old health insurance company. Double health insurance is also excluded. The Social Security Code regulates all of this in the same way and in a binding manner for all health insurance companies.
Do I have to inform my employer about the change of health insurance?
Employees inform their employer informally about the change in health insurance. The employer receives membership confirmation from the new health insurance fund in the electronic notification procedure. Those who are unemployed inform the employment agency, pensioners the pension insurance institution.

Who still has to cancel health insurance?
If you want to leave the statutory health insurance system, you still have to cancel your health insurance, for example, because you want to take out private insurance or move abroad.
Do treatments that have already been started continue when I change my health insurance provider?
The health insurer must approve some medical treatments before they begin. If a treatment approved by the old health insurance company has not yet been started, you must reapply to the new health insurance company. If you have already begun an approved treatment, the new health insurance company will cover the cost of further treatment. You should inform the new health insurance company immediately after joining the ongoing treatment. As a rule, you will have to return aids such as wheelchairs and receive an equivalent replacement from the new health insurance company. In the case of medications, it is also conceivable that you will receive other equivalent medications.
THE HEALTH INSURANCE CHANGE STEP BY STEP
STEP 1: FIND A SUITABLE NEW HEALTH INSURANCE COMPANY
Think about which health insurance company best suits your needs. Our health insurance comparison calculator will help you. Recommendations from friends, relatives, or colleagues are often helpful: Who has had good experiences with which health insurance company?
STEP 2: APPLY FOR MEMBERSHIP
Apply for membership to your new health insurance company. You can request the application form from the health insurance change service or change it online. Note: The entry date and the name of the previous insurance company are required for processing your application. By the way: If you are already a statutory health insurance fund member, you have a right to switch. The new health insurance company you choose must accept you – regardless of age or health status.
STEP 3: INFORM EMPLOYER, EMPLOYMENT AGENCY, OR PENSION INSURANCE COMPANY
As soon as you have received confirmation from the new health insurance company stating the change date, inform your employer about the change of health insurance company. The employer will receive an electronic membership certificate from the new health insurance company. If you are unemployed, inform the employment agency and pensioners to tell the pension insurance provider.
You need to load content from reCAPTCHA to submit the form. Please note that doing so will share data with third-party providers.
More Information


